In this article:
When we think of the digestive tract, the gallbladder is often an afterthought compared to the better-known organs like the stomach or intestines. The gallbladder is essential, as it affects your entire digestion process. When something is wrong with your gallbladder, the signs and symptoms can be pretty obvious…and unpleasant! Gallbladder disease encompasses a range of conditions. The best-known condition is gallstones, which can cause significant abdominal pain and are the reason for over one million emergency room visits annually. Gallbladder removal surgery is one of the most common procedures performed today. Beyond its standalone health implications, gallbladder disease has been increasingly linked to thyroid disorders, particularly autoimmune Hashimoto’s thyroiditis and hypothyroidism. This article explores the symptoms, diagnosis, and treatment of gallbladder disease and its intriguing connection to your thyroid health.
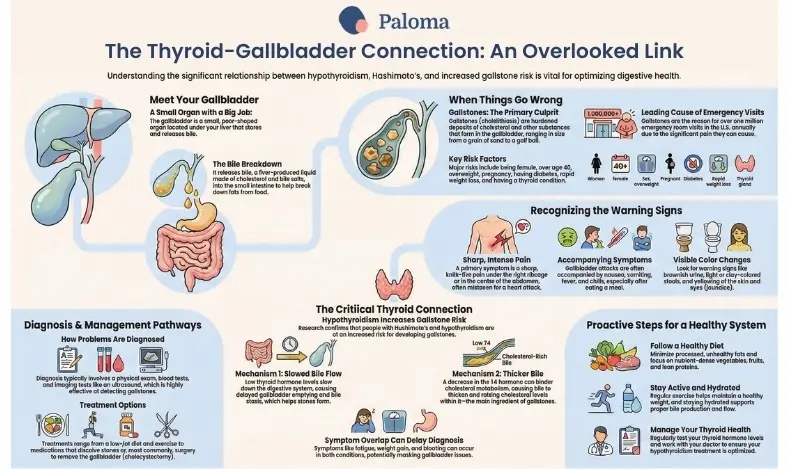
The gallbladder is a small, pear-shaped organ located beneath the liver. The gallbladder’s job is to store bile until the stomach sends hormones, indicating that bile is needed to help break down certain foods. Bile is a liquid substance made by the liver that helps break down fat during digestion. Bile has a greenish color and is comprised of cholesterol, phospholipids, water, and bile salts.
When the stomach signals that food has entered the digestive tract, the gallbladder releases bile down the common bile duct, emptying into the duodenum, the first part of the small intestine.
Sometimes, gallstones (also known by the medical term cholelithiasis) can form in the bile duct from cholesterol and other substances in the bile. Gallstones are hardened deposits (or stones) that can be as small as a piece of sand or as large as a golf ball. You can have just one stone or many. Some gallstones pass without any symptoms; others can cause excruciating pain.
In some cases, the gallbladder becomes inflamed, usually due to the gallstones. This is called cholecystitis. When gallstones become lodged in the bile duct, the condition is called choledocholithiasis and can lead to an infection known as cholangitis.
Gallstones can form for various reasons, but we don’t fully understand the mechanism behind the formation of these stones. Some stones are caused by too much cholesterol or bilirubin. Other times, stones appear because the gallbladder does not empty correctly.
Certain factors increase your risk for gallbladder problems, including:
- Being female
- Being over age 40
- Being overweight or obese
- Lack of exercise
- Pregnancy
- Eating a high-fat, high-cholesterol diet
- Not getting enough fiber
- Having diabetes
- Rapid weight loss
- Being Hispanic or Native American
- A history of liver disease
- Taking certain medications, such as those containing estrogen
- Having a thyroid condition
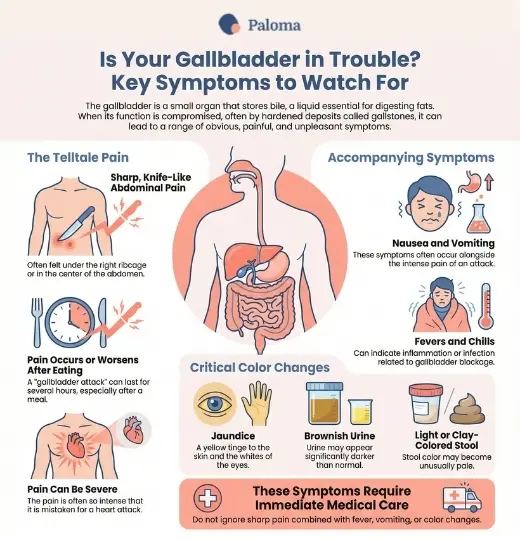
Many people have gallstones and don't have any symptoms, but some people can experience tremendous pain when a stone blocks the bile path. This pain is often described as feeling sharp and almost knife-like under the right ribcage or in the center of the abdomen. Because of its location and the severity of the pain, many people mistake it for a heart attack.
Typically, the pain from gallstones (also referred to as a gallbladder attack) lasts for several hours and is more severe after eating. The timing makes sense because the stomach sends hormones trying to get bile to empty at mealtimes.
Other symptoms can accompany the expected pain of gallstones, including fevers, chills, nausea, and vomiting. Gallstones can also lead to color changes in certain body systems and processes, including:
- Brownish urine
- Light-colored or clay-colored stool
- Yellow-tinged skin and whites of the eyes
Any of these symptoms, coupled with sharp pain, fevers, chills, and vomiting, all require immediate medical care.
Evaluating gallbladder issues involves a combination of medical history, symptom evaluation, physical examination, imaging tests, and blood tests. During the physical examination, the abdomen is palpated for tenderness, focusing on the upper right quadrant, where the gallbladder is located. This helps identify signs of inflammation or pain that might indicate gallbladder problems.
Imaging tests play a crucial role in visualizing the gallbladder and surrounding organs. Ultrasound is typically the first-line imaging test, as it effectively detects gallstones and inflammation. A CT scan may be performed for more detailed imaging, providing comprehensive views of the gallbladder and adjacent structures. A HIDA scan (Hepatobiliary Iminodiacetic Acid) is used to assess the functional capacity of the gallbladder, while MRCP (Magnetic Resonance Cholangiopancreatography) evaluates the bile ducts for potential blockages or abnormalities. ERCP (Endoscopic Retrograde Cholangiopancreatography) is used to diagnose and treat bile duct stones.
Blood tests are also essential in the diagnostic process. An elevated white blood cell count may indicate an infection, while liver function tests can reveal signs of bile duct obstruction. Additionally, measuring pancreatic enzyme levels helps rule out pancreatitis, which can sometimes present with similar symptoms to gallbladder issues. Together, these diagnostic tools provide a comprehensive assessment of gallbladder health and guide appropriate treatment strategies.
Treatment for gallbladder disease varies depending on the severity and type of the condition. For mild cases, lifestyle modifications are often the first line of defense. Adopting a low-fat diet can help reduce bile production and lower the risk of gallstone formation, while regular exercise further minimizes this risk.
When lifestyle changes are insufficient, medications may be prescribed. Ursodiol, or ursodeoxycholic acid, is commonly used to dissolve cholesterol gallstones. In cases of infection, antibiotics are necessary to manage the condition and prevent complications.
For more severe or complicated cases, surgical interventions are typically required. The most common procedure is a cholecystectomy, which involves removing the gallbladder. This is usually performed laparoscopically, a minimally invasive approach that allows for quicker recovery. However, open cholecystectomy may be necessary for more complex cases. Additionally, endoscopic retrograde cholangiopancreatography (ERCP) is a non-surgical technique that removes bile duct stones.
In rare cases, non-surgical options like lithotripsy may be considered. This shock wave therapy is designed to break up gallstones, although it is infrequently used due to limited effectiveness and availability. Each treatment option is tailored to the patient’s condition and overall health needs.
For some time, we have known there is a relationship between hypothyroidism and gallbladder disease. Research has confirmed this relationship. For example, a 2018 study reported that people with Hashimoto’s thyroiditis (the autoimmune condition that is the primary cause of hypothyroidism) are at an increased risk for gallstones and gallbladder removal.
The autoimmune nature of Hashimoto’s thyroiditis also plays a role in gallbladder health. Individuals with one autoimmune disorder have an elevated risk of developing other autoimmune conditions, including those affecting the biliary system. The chronic inflammation associated with autoimmune thyroiditis may worsen gallbladder inflammation, while thyroid hormones influence bile composition and gallbladder motility.
A slowed thyroid gland, a common result of Hashimoto’s thyroiditis, can significantly impact the digestive system, leading to a slowdown in bile flow and gallbladder emptying. A study published in the journal Surgery found that hypothyroidism may result in delayed emptying of the biliary tract. This slowed emptying can contribute to the formation of gallstones and gallbladder inflammation. Some sources suggest that thyroid hormones may affect bile composition, thus interfering with its natural ability to flow without blockage. A decrease in T4 (thyroxine) may hinder cholesterol metabolism in the liver, causing bile to thicken. Recall that cholesterol is one of the main components of gallstones. In addition, the altered lipid metabolism associated with hypothyroidism can increase cholesterol levels in bile, further predisposing individuals to gallstone formation.
Even subclinical hypothyroidism can impact gallbladder function and increase the risk of gallbladder disease. The reduced levels of thyroid hormones lead to decreased gastrointestinal motility and bile stasis, contributing to an environment conducive to gallstone formation. Additionally, hypothyroidism raises cholesterol levels in bile, further promoting the development of gallstones.
Another critical aspect of the relationship between hypothyroidism and gallbladder function is the decreased gallbladder contraction in response to cholecystokinin, a hormone that stimulates bile release. This diminished response can further contribute to bile stasis and gallstone formation.
It’s worth noting that the symptoms of hypothyroidism, such as fatigue, weight gain, and bloating, may overlap with or mask the symptoms of gallbladder disease, potentially leading to delays in diagnosis. This overlap underscores the importance of comprehensive evaluation and consideration of both thyroid and gallbladder function in patients presenting with these symptoms.
Overall, the relationship between gallbladder disease and autoimmune Hashimoto’s thyroiditis is multifaceted, involving various physiological mechanisms. Understanding these connections is crucial for healthcare providers in the diagnosis and management of patients with thyroid dysfunction and potential gallbladder issues.
Based on the risk factors above, you will see that there are certain risk factors that you cannot change. However, you may be able to change many risk factors with lifestyle adjustments.
One of the best things you can do to improve your gallbladder (and overall) health is to follow a healthy diet that includes good sources of protein, healthy fats, and nutrient-dense vegetables and fruits. We know a high-fat diet significantly contributes to gallstones, so minimizing processed, unhealthy fats in your diet is a good first step.
You’ll also want to stay hydrated because adequate water intake supports bile production and flow.
Simultaneously, being sedentary, and to that extent being overweight and obese, increase your risk. Regular exercise and increasing your daily movement can help improve your weight profile. Even opting to carry your groceries, walk the dog, or sweep the sidewalk can all increase your non-exercise activity thermogenesis (NEAT) to support a healthy weight and metabolism.
Finally, because gallstones positively correlate with hypothyroidism, regularly checking your thyroid hormone levels is important. Thyroid disease can appear at any point in a person’s life, but it is more common in women, people over age 50, and those with a family history of thyroid disease. If you have pre-existing hypothyroidism, it’s crucial to optimize your treatment to ensure peak thyroid function.
Testing your thyroid is easy with the Paloma at-home thyroid test kit, and follow-up with a doctor specializing in hypothyroidism and Hashimoto’s is at the tip of your fingers. Treating thyroid disease can help improve numerous other symptoms and ward off other health conditions, including gallstones.
Gallbladder disease presents a spectrum of challenges, particularly for individuals with thyroid disorders like Hashimoto’s thyroiditis and hypothyroidism. Understanding the complex interplay between thyroid health and gallbladder function is critical for timely diagnosis and effective treatment. By addressing both conditions comprehensively and proactively managing risk factors, you can achieve better overall health and quality of life.
Paloma Health members can work with thyroid-savvy practitioners to ensure that hypothyroidism treatment is optimized, which – along with significant lifestyle changes – can help reduce your risk of gallbladder disease.
- The gallbladder stores and releases bile, a vital digestive liquid produced by the liver, to aid in breaking down fats. Dysfunction can lead to painful symptoms and complications like gallstones.
- Gallstones, formed from cholesterol and other bile substances, are a common cause of gallbladder disease, often requiring surgical removal or other interventions.
- Risk factors for gallbladder issues include obesity, high-fat diets, rapid weight loss, certain medications, and conditions like diabetes or hypothyroidism.
- Hypothyroidism and Hashimoto’s thyroiditis are strongly linked to gallbladder disease due to their impact on bile flow, bile composition, and gallbladder motility.
- Symptoms of gallbladder problems include sharp pain under the ribcage, nausea, bloating, jaundice, and fever, often requiring immediate medical attention.
- Diagnosis involves a combination of medical history, physical exams, imaging tests like ultrasounds or CT scans, and blood tests to assess inflammation and bile duct function.
- Maintaining a healthy diet, regular exercise, proper hydration, and optimal thyroid hormone levels are key strategies for reducing the risk of gallbladder disease and its complications.

.webp)

.webp)











